Vulvar ulcers are often very painful sores with red and swollen areas surrounding them, leading to dysuria or even prevent urination altogether if left untreated, and may become infected without treatment.
CUPERTINO, CALIFORNIA | NOW THEN DIGITAL — Vulvar ulcers can be caused by any number of factors, including infections and allergic reactions. You can help protect yourself by practicing safe sexuality, using barrier protection during sexual activity and keeping the area clean.
Your doctor can diagnose vulva ulcers through asking questions, performing physical exams and lab tests. If the cause of the ulcers is an infection, antibiotics or antivirals will likely be prescribed as treatment.
Vulvar ulcers, when untreated, can lead to infection and complications like fever or severe infections. Scarring, discoloration, and reduced skin elasticity can result.
General Information
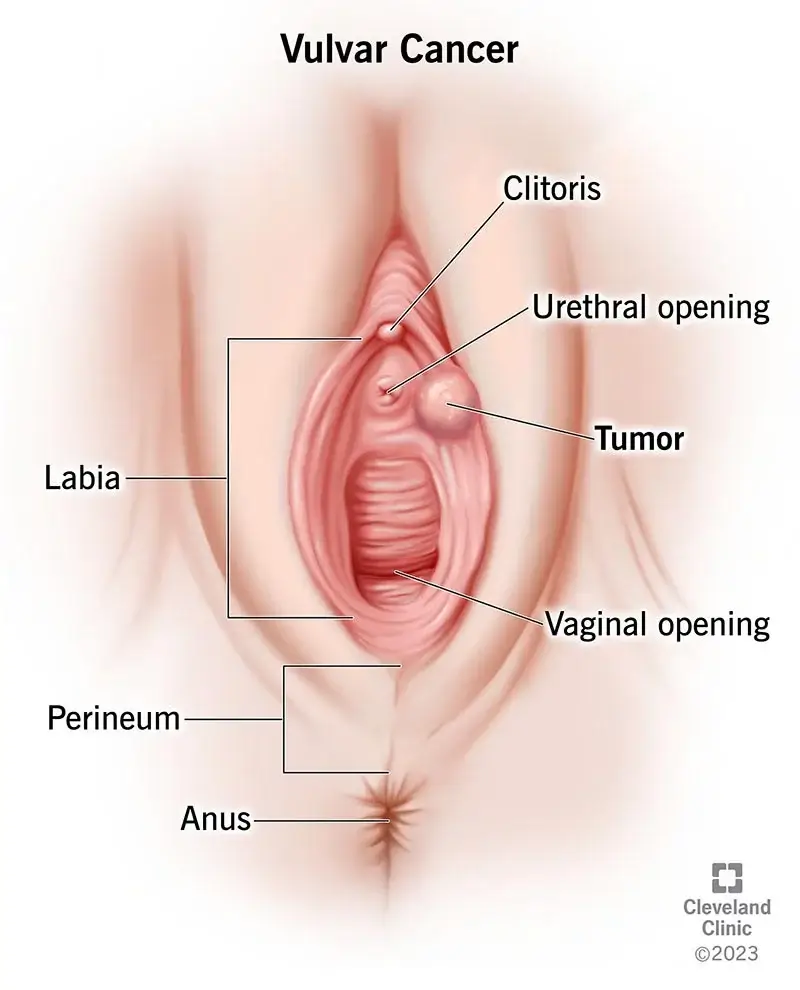
Ulcers in the vulva are typically painful (or itchy) sores that form on the vulva or perianal skin, usually on either end of the cervix.
Vulvar ulcers may be caused by herpes simplex virus (HSV), sexually transmitted infections like HPV and nonsexually transmitted infections like aphthous ulcers of the vulva (APOHTHOUS ulcers of the VULVA), granuloma inguinale or Molluscum contagiosum.
Additionally autoimmune diseases like systemic Lupus Erythematosus may also result in itchy but painless sores in this area of skin.
Vulvar ulcers may also result from allergic reactions to soaps, body wash or shaving products; conditions like psoriasis or eczema in the perianal skin; poor hygiene practices; medical treatments like diaphragms or pessaries used for medical treatments like incontinence management or pessaries used as contraception devices; as well as medications like antibiotics and corticosteroids – though cancerous vulvar ulcers are quite rare.
Accurate diagnosis of vulvar ulcers involves conducting a comprehensive medical history review and physical exam, in addition to laboratory testing such as blood or swab cultures for viral/bacterial infection, urine analysis tests and even possibly extracting part of an ulcer sample for further analysis with PCR or culture techniques.
Symptoms
Vulvar ulcers, appearing on the vulva, vary in severity and cause pain. Untreated ulcers risk infection, demanding medical care.
Diagnosis involves symptom review and a physical exam. Doctors check for redness, swelling, blisters, and sores. Testing may identify STIs like herpes, using swabs and urine samples.
STIs such as herpes simplex, HSV, herpes B, and STI-caused genital warts lead to vulvar ulcers. Nonsexual factors encompass infections, physical injury, and autoimmune diseases like Behcet’s or pemphigus vulgaris.
Non-STI contributors involve inflammatory bowel diseases, chemical exposure, hormone shifts (menopause), and allergic reactions (contact dermatitis).
Certain STIs cause cancer; e.g., HPV causes 69% of vulvar cancers. In 2017, the U.S. saw 5,416 vulvar cancer cases, with higher risk in white females.
Untreated chlamydia and gonorrhea may lead to pelvic inflammatory disease (PID), causing fertility issues (1 in 8 females with PID) as per the CDC.
Untreated STIs linked to vulvar ulcers can lead to serious complications, infertility (24,000 cases yearly), and increased HIV risk.
Causes
Vulvar ulcers may be caused by sexually transmitted diseases (STDs), such as herpes, genital warts, chancroid and syphilis. These STDs cause painful fluid-filled sores in the vaginal area as well as fever, swollen lymph nodes or rash symptoms – typically treated using antiviral or antibiotic medications.
Other causes of vulvar ulcers may include reactions to certain medicines, like steroids, and autoimmune conditions like Behcet’s disease. Vasculitis – inflammation of blood vessels within the vascula – can also contribute to these ulcers and is more prevalent among women who take certain drugs or have an underlying illness.
Doctors usually utilize standard tests to diagnose vulvar ulcers, including blood, urine and swab samples to look for infections as well as CT or ultrasound scans if they suspect a more serious underlying issue; good sexual hygiene and using protection during sex can often help avoid sores as well as STDs.
Vulvar ulcers may develop as a reaction to chemicals found in bath or washing products, itchy genital skin or shaving/waxing abrasions. Contact dermatitis due to nickel, poison ivy or perfume allergies can also trigger them. Vulvar ulcers are often very painful sores with red and swollen areas surrounding them, leading to dysuria or even prevent urination altogether if left untreated, and may become infected without treatment.
Diagnosis
Vulvar ulcers are typically diagnosed by conducting a physical exam and collecting a sample to look under a microscope for signs of inflammation or infection.
A sample may also be sent for PCR testing to identify specific viruses or bacteria present, while in more serious cases a CT scan or MRI may be requested to assess deeper tissue involvement.
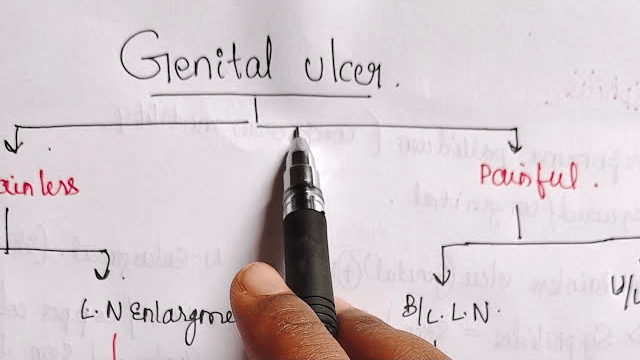
Genital ulcers can be the result of sexually transmitted diseases (STDs), but they can also occur as rare sequelae from autoimmune conditions, trauma or drug interactions. Herpes, shingles and syphilis infections have also been known to cause them.
Skin conditions like lichen planus, psoriasis and erythema multiforme can all increase the likelihood of vulvar ulcers in women.
Women experiencing itching and burning sensations from these ulcers typically also exhibit scaley or scabby patches on their vaginum; treatment often includes topical or oral medications to relieve itching, inflammation and promote healing; in some cases a doctor may suggest sterilizing with povidone-iodine solution or another antiseptic agent to ensure healing takes place more effectively.
A doctor will also ask patients about symptoms like pain, red bumps or sores that ooze or bleed, swelling or tenderness in an area, discharge from lesions, itching, discharge from lesions and itching sensations. He or she will also check for conditions like autoimmune skin disorders, lichen planus or certain medications.
Treatment
Women’s vulva skin is particularly delicate, so even products that usually cause no adverse reaction elsewhere may irritate this delicate area and lead to ulcerative lesions.
Scratching or rubbing too frequently in this area may also irritate it and lead to lesions forming; other causes for vulvar ulcers include herpes and syphilis infections, parasitic infestation such as genital lice and autoimmune illnesses like psoriasis or lichen planus.
Vulvar ulcer treatments depend on the cause:
1. Medications:
– Anti-inflammatories like ibuprofen.
– Topical anesthetics (lidocaine).
– Corticosteroids.
– Antihistamines.
– Antivirals for viral infections.
– Antibiotics for bacterial infections.
– Immunomodulatory drugs like methotrexate.
2. Topical:
– Barrier ointments (petroleum).
– Steroid creams.
3. Pain Relief:
– Warm baths.
– OTC pain relievers.
– Oral or topical analgesia.
4. Hygiene and Care:
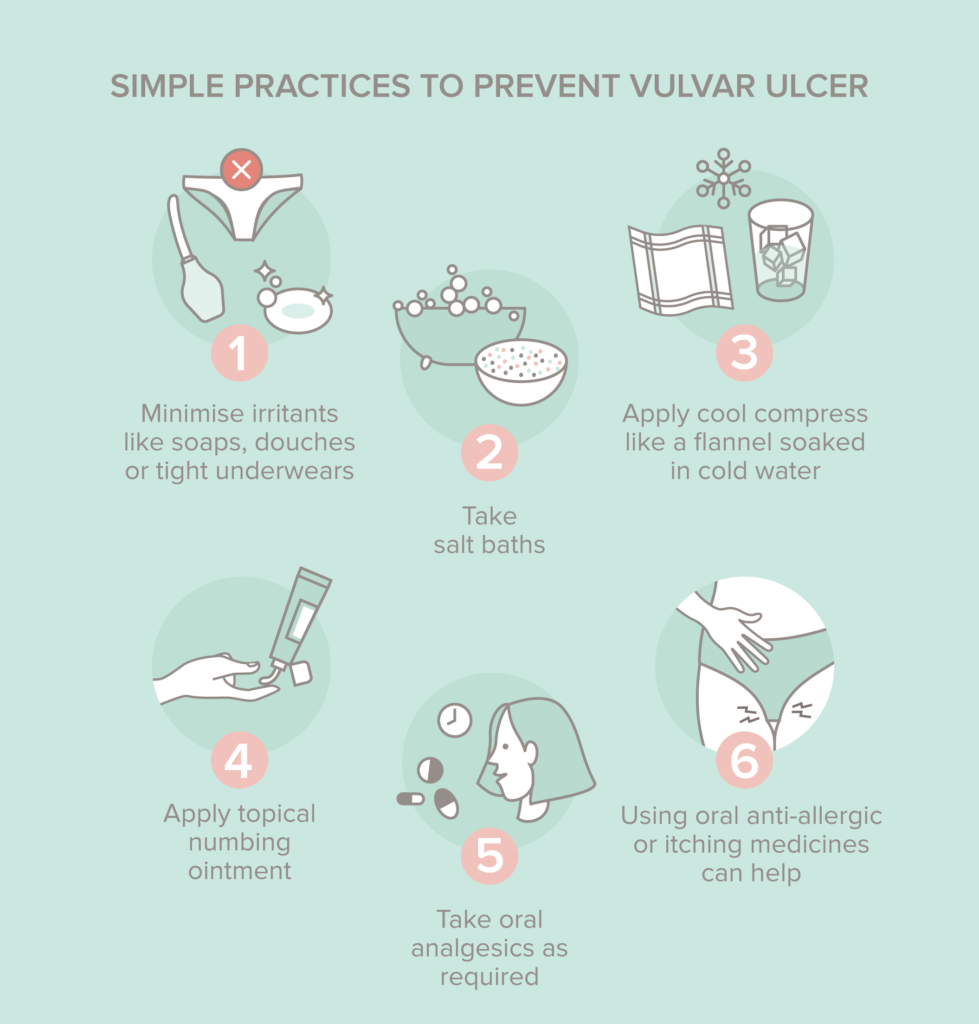
– Avoid irritants (soaps, tight clothing).
– Maintain hygiene for recovery.
Consult a healthcare provider for proper diagnosis and tailored treatment. Tests like exams, blood tests, or biopsies aid in diagnosis, guiding suitable treatment choices.

Other medical conditions, like tuberculosis, can also contribute to vulvar ulcers as well as fever and malaise symptoms.
Treatment options for such disorders can include medication to suppress immune systems and reduce inflammation in affected areas; antiviral drugs for herpes infections as well as antibiotics can also be used; topical medications or steroids may help inflammatory conditions like contact dermatitis be treated; while surgical interventions may also be required depending on its source and can range from simple to complex procedures aimed at solving its source.
If a virus is the source of vulvar ulcers, a doctor will typically prescribe antiviral medicine to combat infection. Otherwise, treatment options to manage disease or injury will likely include medications like an antacid to ease discomfort from peptic ulcer disease; or advice such as wearing loose clothing and practicing good hygiene to avoid further damage may be provided by their provider.
How Long Does It Take for Vulvar Ulcers to Heal
The healing time for vulvar ulcers varies:
– Most heal in 7-14 days (National Association of Pediatric and Adolescent Gynecology).
– Genital ulcers usually take about three weeks but can take up to six (Rapid STD Testing).
– Some may resolve on their own with proper care in a few weeks, while others need prompt therapy (Healthline).
To aid healing, minimize irritants, use analgesia, practice good hygiene, and consult a healthcare provider for diagnosis and treatment.
Editor’s Note: Please contact press@nowthendigital.com if you find any of the content to be inaccurate or outdated.
You’re reading nowthendigital.com — which breaks the news about Uganda, Kenya, Nigeria, South Africa and the rest of the world, day after day. Be sure to check out our homepage for all the latest news, and follow NOW THEN DIGITAL on YouTube, Google, Web Stories, Google News, Medium, LinkedIn, Twitter, Reddit, Pinterest, Linktr, Buy Me a Coffee, Truth Social, and Flipboard to stay in the loop.