Rheumatoid arthritis, also known as RA, is a condition where the immune system mistakenly attacks healthy cells in the body. This leads to inflammation and painful swelling in the affected areas.
CUPERTINO, CALIFORNIA | NOW THEN DIGITAL — Painful joints often experience tenderness, stiffness and inflammation from arthritis – symptoms which may come and go periodically or remain constant over time.
Medicine may help reduce symptoms and prevent joint damage. You could try antimalarial medicines (e.g. hydroxychloroquine), leflunomide, methotrexate or biologics; physical or occupational therapy could also provide support.

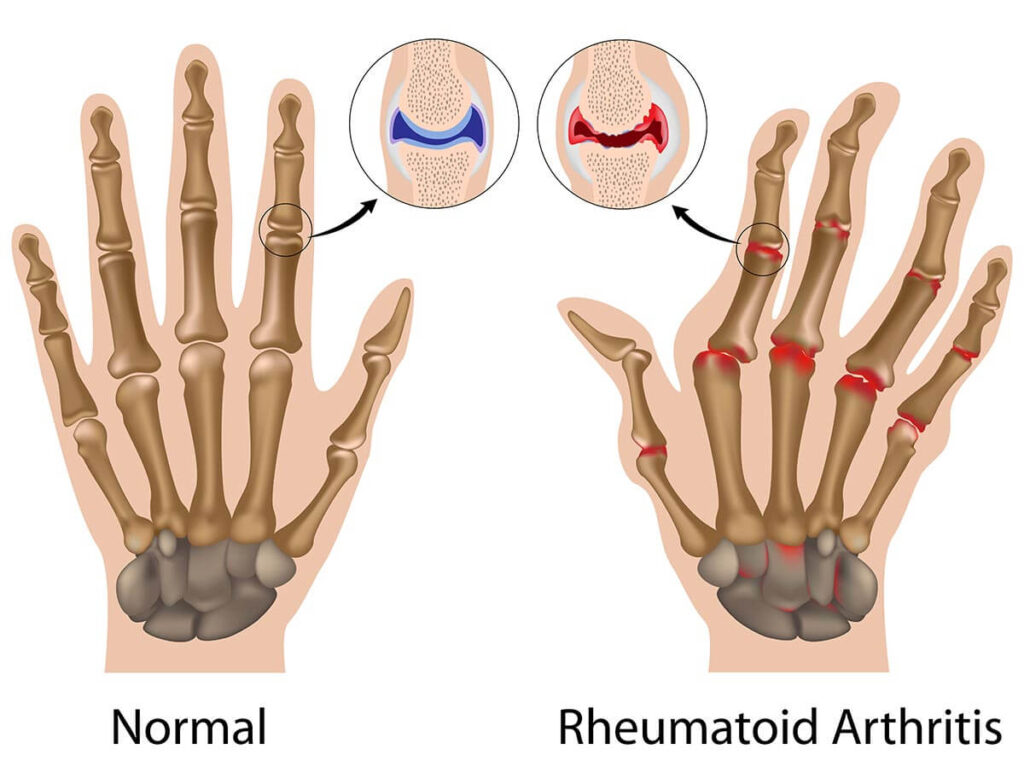
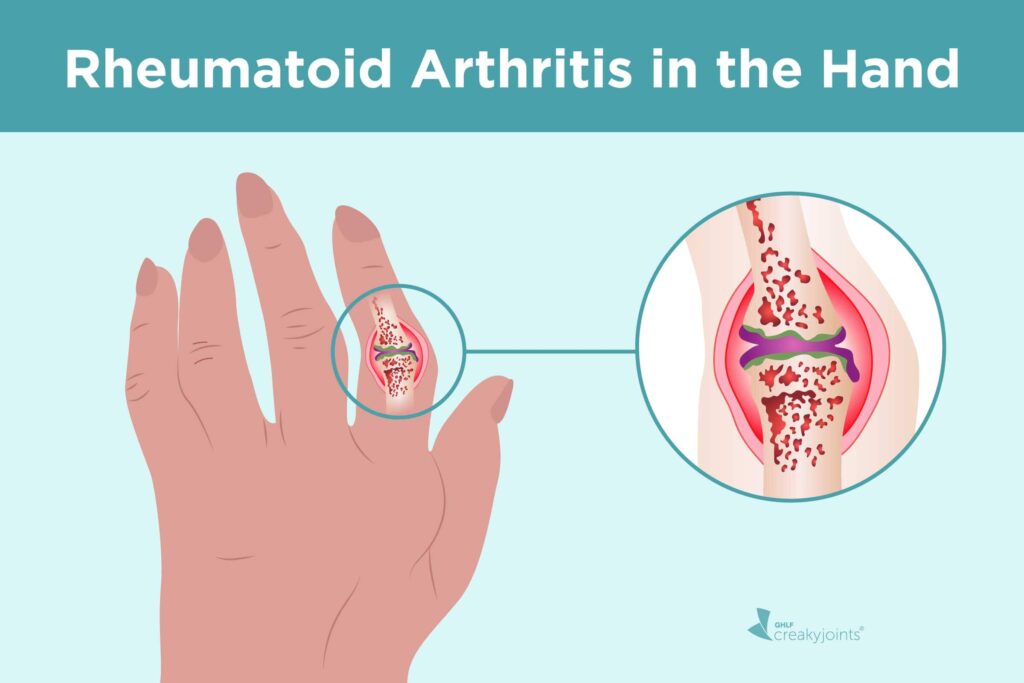
Rheumatoid arthritis occurs when the immune system attacks healthy tissue in and around joints inadvertently, leading to ongoing inflammation and pain. Over time, this inflammation may damage cartilage — the soft cushion between bones that allows easy joint movement — as well as deform joints and cause pain or even destroy them altogether.
What is Rheumatoid Arthritis?
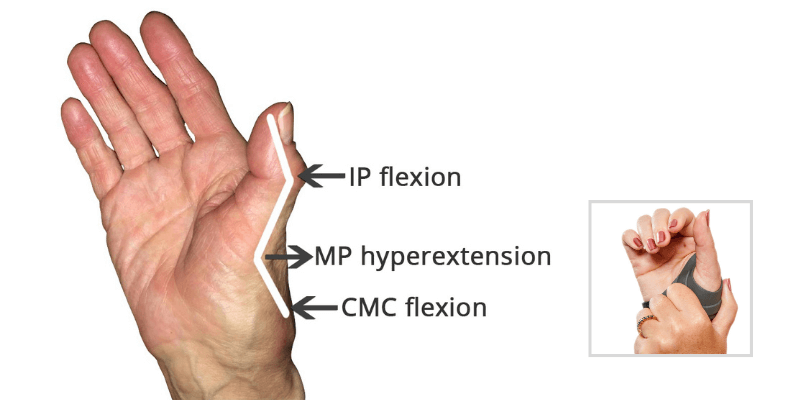
Rheumatoid Arthritis (RA) is a progressive chronic condition. It can impact many joints throughout your body, from small ones such as in the hands and feet to larger ones like spine. Over time it weakens muscles and tendons before damaging cartilage – the protective tissue covering bones in joints.
Your doctor will diagnose RA based on symptoms as well as physical exam. In addition, blood tests and imaging tests may also be ordered.
X-rays and magnetic resonance imaging (MRI) can detect early joint damage. Both methods depict changes to the shape and areas of swelling. Palpation may help your doctor distinguish spongy joint inflammation from firm, knobby bony expansions of an affected bone.
Symptoms
People living with RA often experience joint pain, swelling and stiffness in the hands, wrists, elbows, knees and feet. Swelling is typically bilateral; that is if one hand or knee is affected then both will also be affected symmetrically by swelling. Swelling can sometimes appear doughy or spongy compared to osteoarthritis’ firm knobby enlargement of joints.
As RA progresses, cartilage in the joints can wear away and bone damage occurs – leading to permanent joint damage without treatment.
People living with RA may also experience flare-ups where symptoms worsen; those in need can prevent their symptoms worsening by following an anti-inflammatory diet plan.
“Typically, morning stiffness is part of it, so they tend to get up in the morning, it feels like, ‘I can’t get moving, it takes me an hour to get moving.’ Fatigue is another sign of it, joint swelling,” said Dr. Sadia Khan M.D., a rheumatologist with Rheumatology at Mercy Medical Center in Baltimore.
Causes
Rheumatoid arthritis occurs when your immune system, normally used to fight infection, mistakenly attacks cells that line your joints instead. This leads to inflammation which swells, stiffens and eventually damages both cartilage and nearby bone over time.
Your doctor will conduct tests and review symptoms to diagnose RA. Additionally, an X-ray or ultrasound may be ordered in order to view how your bones and joints appear.
Medication may help ease pain and slow joint damage. Such medications include nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids.

Risk factors
Combinations of genes and non-genetic factors increase your risk for rheumatoid arthritis (RA). People who have a family member with this condition are at increased risk, while genes can make you more or less prone to it by altering how your immune system recognizes proteins within your own body as well as bacteria invasion.
Smoking significantly increases your risk for RA, particularly if you possess certain HLA shared epitope markers. Being female increases that risk further; estrogen may play a part in this connection.
Studies show that RA is more likely to occur after major shifts in hormone levels, such as after childbirth or menopause. Some experts believe these fluctuations in hormonal balance could trigger your genetically predisposed immune system into turning against itself and creating inflammation.
Treatment
Thanks to recent advances in treatment, it’s much less common for people living with RA to progress to more serious stages. By getting diagnosed early and following your prescribed treatments, you can reduce pain and stiffness as well as prevent permanent damage to joints or other parts of the body, keeping symptoms from worsening over time.
Medication that changes how the immune system works can help to stop or delay joint damage. Examples include DMARDs and biologic medicines like tumor necrosis factor inhibitors; TNF inhibitors; Janus Kinase Inhibitors like Tofacitinib (Xeljanz), Baricitinib (Olumiant), and Upadacitinib (Rinvoq) are now widely available through NHS services.
Other medications can provide relief from eye problems, fatigue and other symptoms of RA. Lifestyle modifications – such as eating healthily and exercising regularly as well as stopping smoking – may also be helpful.
Uncommon Signs of Rheumatoid Arthritis
Rheumatoid arthritis (RA), an autoimmune arthritis, strikes with joint pain, swelling, and stiffness. Yet, RA sneaks beyond joints, bringing forth diverse symptoms. These are known as extra-articular manifestations.
Witness the unusual symptoms of rheumatoid arthritis:
- Hearing troubles: RA targets the neck and jaw joints, welcoming sleep apnea. Consequently, daytime exhaustion, disrupted sleep, and snoring emerge from blocked airways during slumber.
- Skin rash and bruises: Besides inflamed and heated joints, RA sufferers sometimes endure skin issues like rashes, discoloration, and fragile bruising.
- Breathing woes: RA ignites lung inflammation, provoking breathlessness, coughing, and chest discomfort.
- Numbness and tingling: Nerve damage befalls RA patients, numbing, tingling, and burning their hands and feet.
- Gum disease: RA provokes gum inflammation, fueling gum disease and tooth loss.
- Escalating body fat: As RA advances, muscles waste away and body fat accumulates, amplifying the cardiovascular threat already lurking in RA patients.
- Irritated eyes: RA inflames the eyes, causing redness, dryness, and irritation.
- Sleep disturbances: RA pain and unease hinder peaceful slumber.
- Mental health woes: RA fosters depression, anxiety, and other mental maladies.
- Cognitive lapses: RA inflicts cognitive impairment, muddling memory, focus, and decision-making.
Note that these symptoms may arise from other sources, necessitating consultation with a physician. Moreover, RA management demands proper treatment to shield joints and subdue extra-articular manifestations.
Options encompass nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), corticosteroids, biologic response modifiers, and lifestyle adjustments like smoking cessation, gentle exercise, weight loss, dietary modifications, and collaboration with a physical therapist.
“I think one of the important things to understand is that rheumatoid arthritis is a chronic inflammatory autoimmune disease. It affects women two times more often than men, often in their childbearing years. So that means that it’s very important that women, but also men, understand pregnancy planning,” says Ashima Makol, M.D., a rheumatologist at the Mayo Clinic in Rochester, MN.
Frequently Asked Questions about RA
1. What is rheumatoid arthritis (RA)?
- Rheumatoid arthritis, also known as RA, is an autoimmune and inflammatory disease characterized by the immune system mistakenly attacking healthy cells in the body, leading to painful inflammation in various parts of the body, primarily targeting the joints.
2. Which parts of the body does RA commonly affect?
- RA mainly targets the joints, often affecting multiple joints simultaneously. The hands, wrists, and knees are commonly affected by this condition, resulting in inflammation of the joint lining and potential long-lasting pain, lack of balance, and deformities.
3. How can one identify the signs and symptoms of RA?
- The signs and symptoms of RA include pain or aching in more than one joint, stiffness in multiple joints, tenderness, and swelling in various joints. Additionally, the symptoms may be observed on both sides of the body, such as in both hands or both knees. Other symptoms can include weight loss, fatigue, weakness, and fever.
4. What causes rheumatoid arthritis?
- The specific causes of RA remain unknown; however, it is an immune response where the body’s immune system mistakenly attacks its own healthy cells, resulting in inflammation and damage to joint tissue.
5. What are the risk factors associated with RA?
- Several factors can increase the risk of developing RA. These include age, with the likelihood of RA increasing as one grows older, and gender, as new cases are more common in women than men. Additionally, genetics play a role, with certain HLA class II genotypes predisposing individuals to the disease. Smoking, history of live births, early-life exposures, and obesity also contribute to an increased risk of RA.
6. How is RA diagnosed?
- RA is diagnosed through a combination of symptoms review, physical examination, and various tests, including X-rays and lab tests. Early diagnosis, preferably within six months of symptom onset, is crucial to initiate treatment and manage the disease’s progression effectively.
7. Who should diagnose and treat RA?
- RA should be diagnosed and treated by doctors or a team of specialists who specialize in caring for RA patients. These specialists, known as rheumatologists, can differentiate RA from other inflammatory joint diseases and provide appropriate care and treatment.
8. How is RA treated?
- RA can be effectively treated and managed through the use of medications, such as disease-modifying antirheumatic drugs (DMARDs) and biological response modifiers (biologicals). In addition to medication, self-management strategies are essential in reducing pain and disability associated with RA.
9. What are the potential complications of RA?
- RA can lead to various physical and social consequences, negatively impacting one’s quality of life. Complications may include premature heart disease, obesity-related health issues, and difficulties with employment due to reduced physical capabilities.
10. How can one manage RA and improve their quality of life?
- Managing RA involves multiple strategies to enhance quality of life. These include engaging in regular physical activity, participating in effective physical activity programs, joining self-management education classes, quitting smoking, and maintaining a healthy weight. These measures can alleviate symptoms and promote a better quality of life for individuals with RA.
Editor’s Note: Please contact press@nowthendigital.com if you find any of the content to be inaccurate or outdated.