Due to modern treatments, it’s less likely for people with RA to reach its advanced stages; however, early diagnosis and compliance with prescribed medication remains important for optimal health outcomes.
CUPERTINO, CALIFORNIA | NOW THEN DIGITAL — Treating rheumatoid arthritis improves symptoms and overall well-being. But the goal goes beyond that. Early treatment slows progression, helping to avoid severe joint damage.
The four stages of rheumatoid arthritis: synovitis, pannus, fibrous ankylosis, bony ankylosis.

What is Rheumatoid Arthritis?
Rheumatoid arthritis often starts as nonspecific symptoms such as fatigue, malaise and weakness before quickly progressing to joint pain, tenderness and swelling.
Your doctor may order imaging studies or blood tests to detect joint damage, as well as specific blood tests to check your RA antibodies.
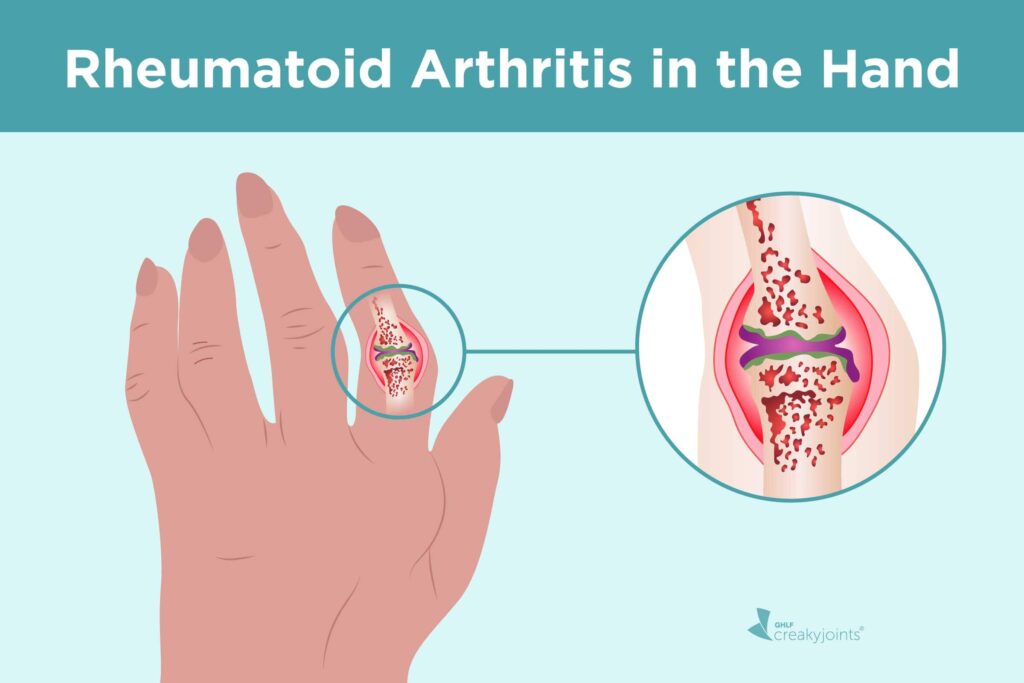
RA affects mostly small joints in your hands and feet, but can also involve larger joints like those found in knees and hips as well as your eyes and lungs. Most cases begin between 30-50 years old but it can happen to anyone regardless of age or gender.
Treatment early can slow the progression of RA and help avoid permanent joint damage and disability. To manage symptoms, start with over-the-counter medicines like Tylenol or nonsteroidal anti-inflammatory drugs like Aleve. Next, consult your physician about prescription options.
Symptoms
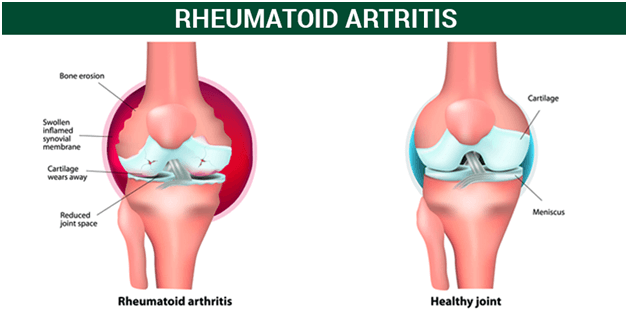
Rheumatoid arthritis causes painful, swollen and stiff joints, often in combination with swelling. As an autoimmune disease, its cause lies with your immune system mistakenly attacking cells lining your joints to cause inflammation that damages both cartilage and joints over time – and other parts of the body, such as your lungs or heart.
RA symptoms may include joint pain and swelling; fatigue; fever; redness in hands and feet, as well as redness and heat in them. Your physician will ask about your symptoms and perform a physical exam; they may order further diagnostic tests such as X-rays, blood tests (erythrocyte sedimentation rate and C-reactive protein), or other tests as needed.
Regular exercise and the balance between activity and rest are proven ways to strengthen joints, reduce pain and fatigue, and keep joints strong. Your doctor can suggest safe exercises, such as walking and mild water aerobics. They may also offer tips to decrease fatigue such as using stairs instead of elevators when possible or parking somewhere that requires extra walking time.
Symptoms of RA may fluctuate over time, especially fatigue. They may also include low-grade fever.
Diagnosis
Diagnosing rheumatoid arthritis early is vital, as early treatment can stop its worsening and reduce permanent damage.
Your doctor will ask about when and how severe your symptoms began; whether they come and go; what makes them better or worse; physical examination; blood testing for inflammation markers like ESR or CRP levels (erythrocyte sedimentation rate or C-reactive protein respectively); as well as ordering blood tests to detect elevated ESR or CRP levels as indicators.
Blood tests may detect antibodies called anti-cyclic citrullinated peptide (anti-CCP), which attack healthy cells in the joints. X-rays and other imaging tests can identify damage to bones, cartilage and ligaments; while additional diagnostic procedures could rule out other conditions that might be contributing to your symptoms – like infectious diseases or cancer.
Since medications used to treat RA may increase your risk of infection, your doctor should monitor for signs of infections as part of treatment.
“I think one of the important things to understand is that rheumatoid arthritis is a chronic inflammatory autoimmune disease. It affects women two times more often than men, often in their childbearing years. So that means that it’s very important that women, but also men, understand pregnancy planning,” says Ashima Makol, M.D., a rheumatologist at the Mayo Clinic in Rochester, MN.

Treatment
Rheumatoid arthritis occurs when the immune system attacks healthy tissue in and around joints inadvertently, leading to ongoing inflammation and pain. Over time, this inflammation may damage cartilage — the soft cushion between bones that allows easy joint movement — as well as deform joints and cause pain or even destroy them altogether.
Your doctor can treat and help manage your symptoms to manage the disease effectively. Lifestyle changes, like losing weight if necessary and exercising regularly (e.g. walking) may help reduce fatigue and build strength more quickly.
They may also suggest heat or cold treatments (like taking a hot shower or sitting in a warm bath); cold helps reduce swelling while heat relaxes tense muscles.
Conventional drugs known as disease modifying antirheumatic drugs or DMARDs can slow the progression of arthritis while protecting tissues. Examples include methotrexate (Trexall, Otrexup and others), leflunomide (Arava) and hydroxychloroquine (Plaquenil).
More recently developed biologic response modifiers may also prove effective, such as abatacept (Orencia), adalimumab (Humira), certolizumab (Cimzia), golimumab (Simponi) and anakinra (Kineret).
What Are the Stages of Rheumatoid Arthritis?
Stage 1: Synovitis
At its root, RA involves inflammation – or synovitis. In this stage, your joints become swollen and stiff with possible cartilage damage; diagnosing early stage symptoms is difficult due to not always showing up on imaging tests such as X-rays.
Symptoms typically begin in your fingers and toes before spreading to larger joints like knees, ankles, hips, or shoulders. They may come and go over weeks or months; worsening during flare-ups could be triggered by stressors like changes to medication, changes to your schedule or other factors.
At times of an attack, symptoms may include joint tenderness or pain that lasts several days, fever, fatigue and the feeling that your heart is racing – all telltale signs. Therefore, treatment must be sought promptly in order to combat such attacks effectively.
At this stage, doctors typically employ low doses of disease-modifying antirheumatic drugs (DMARDs). These medicines block your immune system’s ability to attack healthy tissue and slow or stop its progression; such medications include methotrexate for inflammation reduction as well as those which restrict pathways within immune cells with anti-TNF-a therapy and biologics being other examples.
It may also help if occupational or physical therapy as well as lifestyle modifications such as weight loss and quitting smoking are combined into treatment.

Stage 2: Cartilage Thinning (Pannus)
At this stage, inflammation damages cartilage – the cushiony material that covers and cushions your bones in joints – leading to stiff and sore joints, with difficulty moving them and possible difficulty sleeping on them. Your doctor may administer a health assessment questionnaire or C-reactive protein blood test in order to detect inflammation within your body.
Over time, damaged cartilage may eventually break down completely and reveal exposed bone, known as osteoarthritis. This stage usually affects knees, hips, hands and feet and in people living with rheumatoid arthritis this process usually unfolds gradually over weeks or months with symptoms coming and going; your rheumatologist may recommend physical therapy and other noninvasive therapies as ways of helping prevent further damage.
At this point, you are likely taking both DMARDs (drugs that slow the progression of RA) and other prescription or over-the-counter medicines to treat your symptoms of RA. Your rheumatologist may also suggest biologic response modifiers – medications which block certain immune proteins – for your treatment plan, such as abatacept, adalimumab, etanercept, golimumab, infliximab or tocilizumab.
Ultimately, if the loss of cartilage in your knees reaches this stage, your rheumatologist might suggest surgery as a way back. One option available to them may include autologous chondrocyte implantation – taking healthy cartilage tissue from one part of your bone that does not bear weight and using it to fill any defects.
Stage 3: Joint Damage (Ankylosis)
At this moderate stage, inflammation continues to wear away more cartilage. Bones rub together more closely, narrowing their spaces further apart. Joint pain increases; stiffness may occur after sitting for extended periods or when you wake up in the morning. Over time, symptoms may come and go but usually worsen over time in what’s known as a flare up.
Uncontrolled inflammation can damage cartilage to such an extent that it erodes completely, leaving bones to rub against each other and cause further pain and swelling. At this stage, X-rays and other diagnostic imaging techniques may show increased bone spur growth as well as an increase in enzymes like metalloproteinases that break down cartilage matrix.
By this stage, joints no longer function normally and symptoms become increasingly severe in ankles, knees, hips and elbows. People experiencing this stage can have difficulty walking and climbing stairs while in some instances the bones fuse together into an ankylosis appearance (ankylosis).
RA symptoms in the late stage are more noticeable than previously. Your doctor can easily identify this stage by asking about when and why the symptoms began, whether they come and go, physical exam results showing swelling, warmth, redness and bumps under skin as well as loss of mobility and ordering blood tests such as an ESR/CRP tests to measure inflammation levels.
Stage 4: No Joints (Bony Ankylosis)
At this stage, your joints become stiff and painful, with cartilage wear off at bone ends due to inflammation leading to erosion of bones themselves. Your doctor can diagnose this stage through physical exam and blood tests such as ESR/CRP.
They will also assess reflexes, strength of muscle tone and reflexes; and may order x-rays and ultrasounds if they detect deformed bone structure due to disease progression.
At this stage, symptoms tend to fluctuate. They’re generally worse first thing in the morning and can become more painful with activity. You may also have low-grade fever; fatigue and other nonspecific systemic symptoms like feeling unwell are also prevalent.
At this stage, it’s essential to seek treatment from a rheumatologist who specializes in RA. They will run tests, x-rays and ultrasounds and discuss your symptoms to diagnose its stage and offer treatment plans.
It would also be wise to keep track of symptoms in a journal so your rheumatologist can identify triggers such as infections, smoking, stress or certain foods or medications which could trigger flare-ups of RA – they can offer ways of managing them so they won’t affect life so severely.
Treatment for Rheumatoid Arthritis at Each Stage
The realm of medical experts has discerned four distinct stages in the progression of rheumatoid arthritis, with each phase necessitating its own unique course of treatment.
Below is a comprehensive elucidation of the treatment options corresponding to each stage:
Stage 1: Early RA
During this initial phase, the synovium, the joint lining, undergoes inflammation. The bones remain unharmed, yet the surrounding tissue frequently swells, rendering the joint both rigid and achingly painful. Treatment alternatives for stage 1 RA comprise:
– Nonsteroidal anti-inflammatory drugs (NSAIDs) to mitigate pain and inflammation.
– Disease-modifying antirheumatic drugs (DMARDs) to impede disease advancement and forestall joint damage.
– Corticosteroids to diminish inflammation.
– Adjustments to one’s lifestyle, such as smoking cessation, engaging in low-impact exercise, weight reduction, dietary modifications, and collaboration with a physical therapist.
Stage 2: Antibodies Emerge, and Swelling Aggravates
During this phase, antibodies manifest, exacerbating the swelling. Joint tissues experience heightened inflammation internally.
For instance, in stage 2 RA affecting the hands, an individual may suffer from stiffness and pain in their finger joints and knuckles, which tend to abate with movement. Treatment options for stage 2 RA encompass:
– NSAIDs to alleviate pain and inflammation.
– DMARDs to impede disease progression and preclude joint damage.
– Corticosteroids to reduce inflammation.
– Biologic response modifiers targeting specific components of the immune system responsible for inflammation.
– Lifestyle modifications, including smoking cessation, low-impact exercise, weight reduction, dietary adjustments, and collaboration with a physical therapist.
Stage 3: Manifestation of Symptoms
Throughout this stage, the joint may deform, accompanied by heightened pain and swelling. This deterioration often precipitates reduced mobility and functionality. Treatment alternatives for stage 3 RA include:
– NSAIDs to mitigate pain and inflammation.
– DMARDs to impede disease progression and preclude joint damage.
– Corticosteroids to diminish inflammation.
– Biologic response modifiers targeting specific components of the immune system responsible for inflammation.
– Surgical intervention to repair or replace damaged joints.
Stage 4: Fusion of Joints
In advanced-stage RA, inflammation subsides, yet the damage persists. The joint’s functionality might deteriorate, giving rise to pain, swelling, stiffness, and restricted movement. Treatment options for stage 4 RA involve:
– NSAIDs to alleviate pain and inflammation.
– DMARDs to impede disease progression and preclude joint damage.
– Corticosteroids to reduce inflammation.
– Biologic response modifiers targeting specific components of the immune system responsible for inflammation.
– Surgical intervention to repair or replace damaged joints.
It is crucial to recognize that the experience of rheumatoid arthritis varies for each individual, and symptoms may not emerge until later stages. Rheumatologists adopt a proactive “treat-to-target” approach, employing aggressive treatment strategies until they achieve a specified treatment objective, such as low disease activity.
Consistent follow-up with a rheumatologist, who conducts joint examinations, monitors systemic inflammation levels through blood tests, and assesses functionality, represents the most effective means of ensuring the effective management and prevention of RA progression.
Editor’s Note: If you find any of our content to be inaccurate or outdated, please contact us at press@nowthendigital.com